
Sophia McCarthy
Operations Manager
For those of us that suffer from regular headaches and migraines, there’s nothing worse than waking up in the morning with a throbbing head, blurry vision and exhaustion. As a migraine sufferer myself, I have realised over the years from talking to fellow ‘migraineurs’ just how common migraines really are in women.
Global statistics estimate that migraine affects 20.7% of women, compared to 9.7% of men. It’s believed that this higher incidence rate in women is down to—you guessed it—hormonal differences.
Migraine versus headache
So, what’s the big deal with migraines? Aren’t they just bad headaches?
First of all, don’t ever say to that someone in the depths of a migraine attack—believe me, you’re not helping! Secondly, it’s important to note that while migraines and headaches can share many similarities, there are some key differences in terms of their severity and impact.
While a headache is comprised of nasty overall pain in the head, face or upper back, a migraine attack can be a very unpleasant and scary thing to experience, particularly if you’ve never had one before.
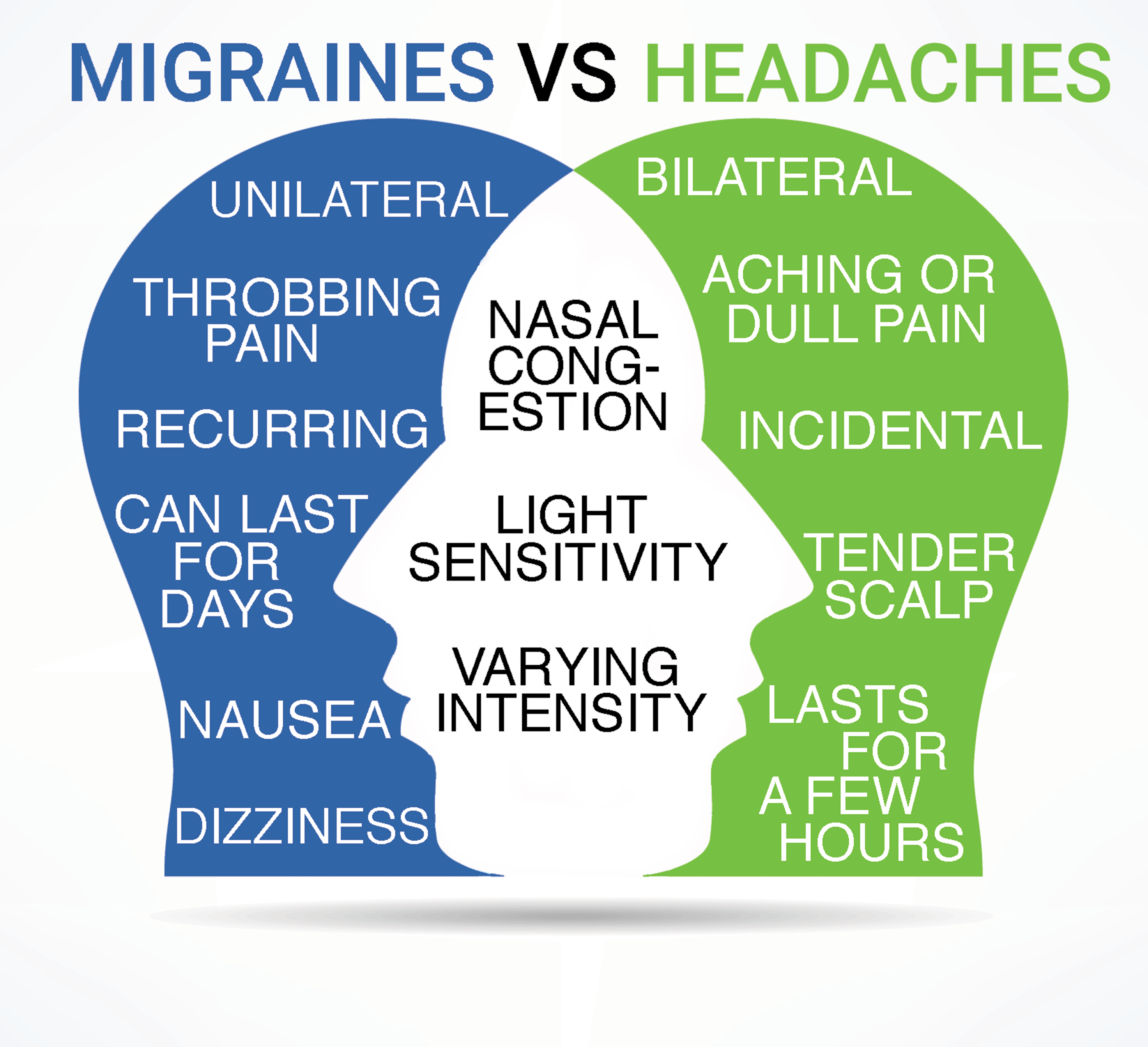
Migraines are characterized by severe pain lasting for multiple days and recurring on a regular basis. Standard headaches typically affect both sides of the brain, whereas migraines more commonly affect only one side. This means that headache tends to be bilateral, while migraines tend to be unilateral. A migraine attack can also last for several days, whereas a headache may only last a few hours and can be treated quite easily with low-grade painkillers. Migraines in comparison can be quite debilitating, forcing the sufferer to lie down in a dark room until the attack has passed.
What actually happens to your brain during a migraine?
A migraine attack is basically when hormones and chemicals trigger a narrowing of the blood vessels in the brain. An article from John Hopkins Medicine provides a more detailed overview of this process:
One aspect of migraine pain theory explains that migraine pain happens due to waves of activity by groups of excitable brain cells. These trigger chemicals, such as serotonin, to narrow blood vessels. Serotonin is a chemical necessary for communication between nerve cells. It can cause narrowing of blood vessels throughout the body.
When serotonin or estrogen levels change, the result for some is a migraine. Serotonin levels may affect both sexes, while fluctuating estrogen levels affect women only.
Some research suggests that when estrogen levels rise and then fall, contractions in blood vessels may be set off. This leads to throbbing pain.
Early signs of a migraine attack
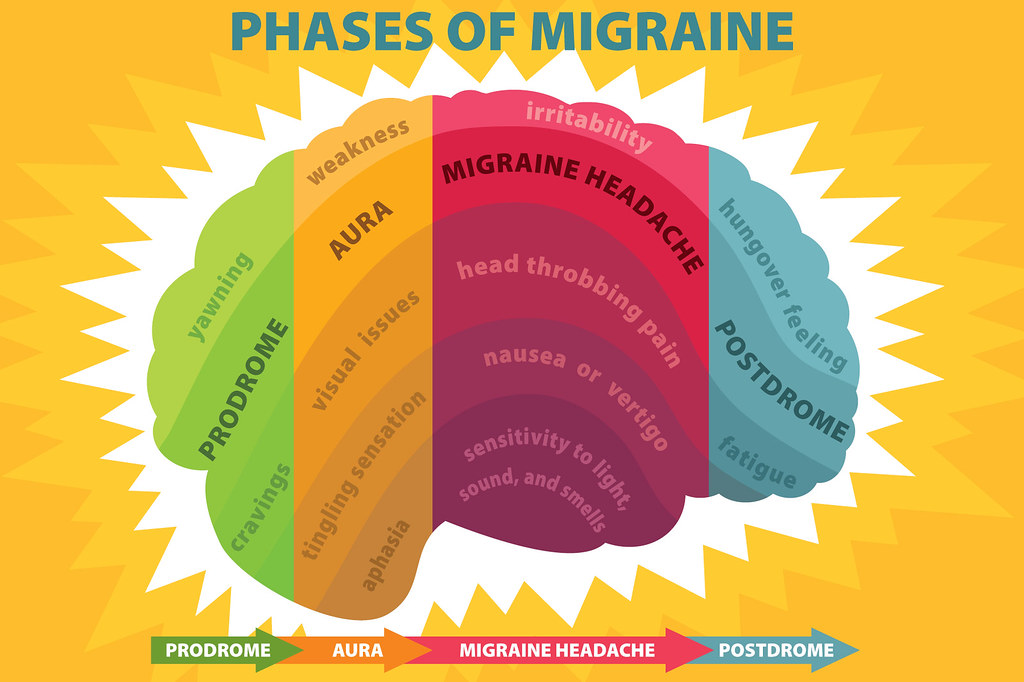
According to the NHS website, the warning signs of an impending migraine can start to appear a few days in advance, such as:
- Feeling very tired and yawning a lot
- Craving certain foods or feeling thirsty
- Changes in your mood
- A stiff neck
- Peeing more
Or you may experience more obvious alarm bells, such as:
- Problems with your sight, such as seeing zigzag lines or flashing lights. This is known as an aura. Aura symptoms should not last longer than an hour. (You should speak to a GP if your vision doesn’t clear after the hour—just to be on the safe side!)
- Numbness or a tingling that feels like pins and needles.
- Feeling dizzy.
- Difficulty speaking.
First-time migraineurs may understandably panic when they have their first aura, as the above aura symptoms are so similar to that of a stroke!
Menstruation Migraine
Now that we have a better understanding as to what a migraine is—what exactly is a menstruation migraine?
A menstruation or hormonal migraine, according the to the NHS, “is most likely to develop in either the 2 days leading up to a period or the first 3 days during a period. This is because of the natural drop in oestrogen levels at these times. The attacks are typically more severe than migraines at other times of the month and are more likely to come back the next day.”
Tips for managing menstruation migraines
So how can these migraines be managed or their severity lessened? While there is sadly is no magical pill to eradicate migraine for good, there are several management options that you can discuss with your GP:
- Medication to regulate hormones, such as an estrogen-only pill to maintain steady estrogen levels, or a low-dosage SSRI to regulate serotonin levels.
- Medications to lessen the severity of attacks, such as Sumatriptan, which works on the serotonin receptors located on blood vessels in your brain, causing them to narrow.
- Exercise and stretching can also help if your migraines are triggered or worsened by tension in the neck and shoulders. Physiotherapy and dry needling may also help with this.
- Don’t go too long without eating. Some doctors theorize that erratic blood sugar levels may increase the chances of a migraine attack.
- Caffeine. This one can be tricky to get right, as small amounts of caffeine have been shown help with migraines (think of over-the-counter headache tablets, such as Exedrin, which contain small amounts of caffeine which speed up the effects of the pain reliever), while too much caffeine can trigger them!
- Magnesium. Magnesium supplements have been shown to help with chronic migraine, as low levels of magnesium seem to cause blood vessels in the brain to narrow, or constrict, which may also play a role in migraine. (WebMD)
- Managing Stress Levels
- Maintaining a Regular Sleep Schedule
- Tracking your migraines. Keeping a migraine diary can be incredibly helpful when figuring out your triggers, especially if they start syncing up with your period.
You should always consult with a GP if your migraines suddenly become more frequent or more painful. There are lots of different factors involved in treating migraine, so don’t suffer in silence!
References and Further Reading
Greater Austin Pain Center: Migraines vs. Headaches: Key Differences You Need to Know
John Hopkins Medicine: How A Migraine Happens
Kelli Yates on Instagram @the.migraine.dietitian
National Library of Medicine: Sex and gender differences in migraines: A Narrative Review
